


17 Fév 20
Why perform spirometry and oximetry in neuromuscular diseases?
Neurological and neurodegenerative diseases are dysfunctions of the central or peripheral nervous system, which, based on the extent and focalization, may manifest themselves in different ways. Nevertheless, they are often severely crippling and sometimes fatal.
Among these is Multiple Sclerosis, a known neurodegenerative disease that affects the central nervous system (brain and spinal cord) with alteration of nerve pulse transmission, and Amyotrophic Lateral Sclerosis (ALS) that affects the cells that control muscle movement. Other diseases may affect the neuromuscular junction (Myasthenia gravis) or the muscles directly (such as muscular dystrophy, polymyositis and dermatomyositis)
In these diseases, involvement of the respiratory muscles causes progressively compromised respiratory function with serious disabilities and shorter survival.
Therefore, in neuromuscular diseases an instrumental pneumological assessment periodically needs to be performed, which includes spirometry and oximetry.
Spirometry in neuromuscular diseases
Among the spirometric parameters, measurement of FVC (Forced Vital Capacity) or SVC (Slow Vital Capacity) allows assessing the extent and following the decline over time of the restrictive defect typical of neuromuscular diseases due to involvement of the respiratory muscles.
The reduction in FVC (and/or SVC) in neuromuscular diseases is also an early indicator of the appearance of hypercapnia (increased carbon dioxide in the blood), further deteriorating the quality of life, as non-invasive assisted mechanical ventilation becomes necessary. When FVC is reduced to below 60%, sleep oximetry needs to be performed annually (see below) and the gases in the arterial blood analysed (blood gas analysis): if the values drop below 40%, much more frequent tests are required.
FVC reduction >20% measured in supine position compared to FVC measured in sitting position is very indicative of weakness of the diaphragm.
Another important spirometric parameter in neuromuscular diseases is PEF (Peak Expiratory Flow) which, related to the indices of expiratory muscle efficiency, may indicate involvement already in the initial stages of these diseases.
Moreover, in the more advanced stages of these diseases, PEF may reveal a compromised coughing mechanism which favours the onset of pneumonia.
In conclusion, these two spirometry parameters – FVC (and/or SVC) and PEF – may for all practical purposes be considered “biomarkers” of the respiratory complications of neuromuscular diseases (in particular, “ventilatory pump defect”).
Oximetry in neuromuscular diseases
Also oximetry plays an important role in therapeutic diagnostic procedures of neuromuscular diseases. In the full-blown stages of these diseases, it is useful to verify the level of respiratory failure in rest conditions.
But, right from the earliest stages, sleep oximetry is important in verifying the outbreak of sleep-related disorders. In fact, it is able to measure prolonged desaturations due to long periods of hypoventilation or hypopnoea during sleep, otherwise measurable only with complex instruments, such as polysomnographs. When prolonged desaturations exceed at least 5 minutes continuously, they are called NOD (Nocturnal Oxygen Desaturation) and can be calculated according to different criteria related to the level of severity. (*1,2,3)
Also NOD severity and duration are predictors of hypercapnia and indicators of the need for non-invasive mechanical ventilation.
In the most advanced stages of neuromuscular diseases, apnoeas also appear during sleep causing rapid desaturations lasting less than 2.5 minutes. Through analysis of these types of desaturation (ODI, Medium Desaturation, Desaturation Peak) and calculation of some parameters, such as the Delta index, the more advanced oximeters are capable of estimating the severity of the apnoeic picture.
In children under the age of 5 years affected by neuromuscular diseases who cannot undergo spirometry or even more complex tests, sleep oximetry at least once a year is recommended.
6-minute walk test (6MWT) in neuromuscular diseases
The 6-minute walk test used in many cardio-respiratory diseases finds little space in the diagnostic setting of neuromuscular diseases. Nonetheless, some of these diseases - such as Multiple Sclerosis - may have partial or complete responses to certain therapeutic and rehabilitation schemes. In these cases, some parameters derived from oximetry analysis performed during the walk test may take on great importance. In particular, DDR4 (Desaturation Distance Ratio - also called Area Under Curve of SpO2/Distance) and O2 GAP5, already important in managing other “restrictive” diseases, such as Pulmonary Fibrosis, where they are also predictors of mortality, can facilitate the comparison of several tests and hence play a role as treatment response indicators. (*4,5)
*
1: desaturations with %SpO2 reduced by at least 4% with respect to the reference value
2: desaturations with SpO2 reduced to below 89%
3: desaturations with SpO2 reduced to below 90% and with a minimum value that drops to below 86%
4: The potential of this index - which depends on the distance covered, the area of desaturation and the recovery time - has been widely demonstrated in patients affected by pulmonary fibrosis.
5: The O2 GAP index represents the estimate of the amount of oxygen (l/min) to be administered to the subject in order to prevent strong desaturation during the walk test.
Conclusions
Compromised respiratory function is one of the most negative moments in the evolution of neuromuscular diseases. Measurement of FVC (and/or SVC) allows in a practical and repeatable way monitoring the evolution of the restrictive defect caused by these diseases and is an early indicator of the appearance of hypercapnia which severely worsens the quality of life with the beginning of mechanical ventilation.
PEF is related to the indices of expiratory muscle efficiency: in the initial stages of neuromuscular diseases, it is an excellent indicator of respiratory muscle involvement while in the more advanced stages it is an indicator of a compromised coughing mechanism which favours the onset of pneumonia.
Therefore, FVC and PEF may for all practical purposes be considered “biomarkers” of the respiratory complications of neuromuscular diseases.
The role of oximetry is not negligible either: if measured at rest, it verifies the onset of full-blown respiratory failure. Sleep oximetry is able to measure prolonged desaturations (NOD), already present in the early stages, and rapid desaturations typical of apnoeic disorders, which, on the contrary, appear in the more advanced stages of these diseases. In addition, some parameters derived from oximetry analysis in the walk test, such as DDR (Desaturation Distance Ratio) and O2 GAP, could be used in certain cases as treatment response indicators.
In conclusion, although some examinations, such as respiratory muscle strength tests, arterial blood gas analysis and polysomnography remain fundamental in some particular conditions, spirometry and oximetry, also in the modern perspective of “minimum assistance levels”, can play an acceptable front-line role in diagnosis and follow-up of neuromuscular diseases.
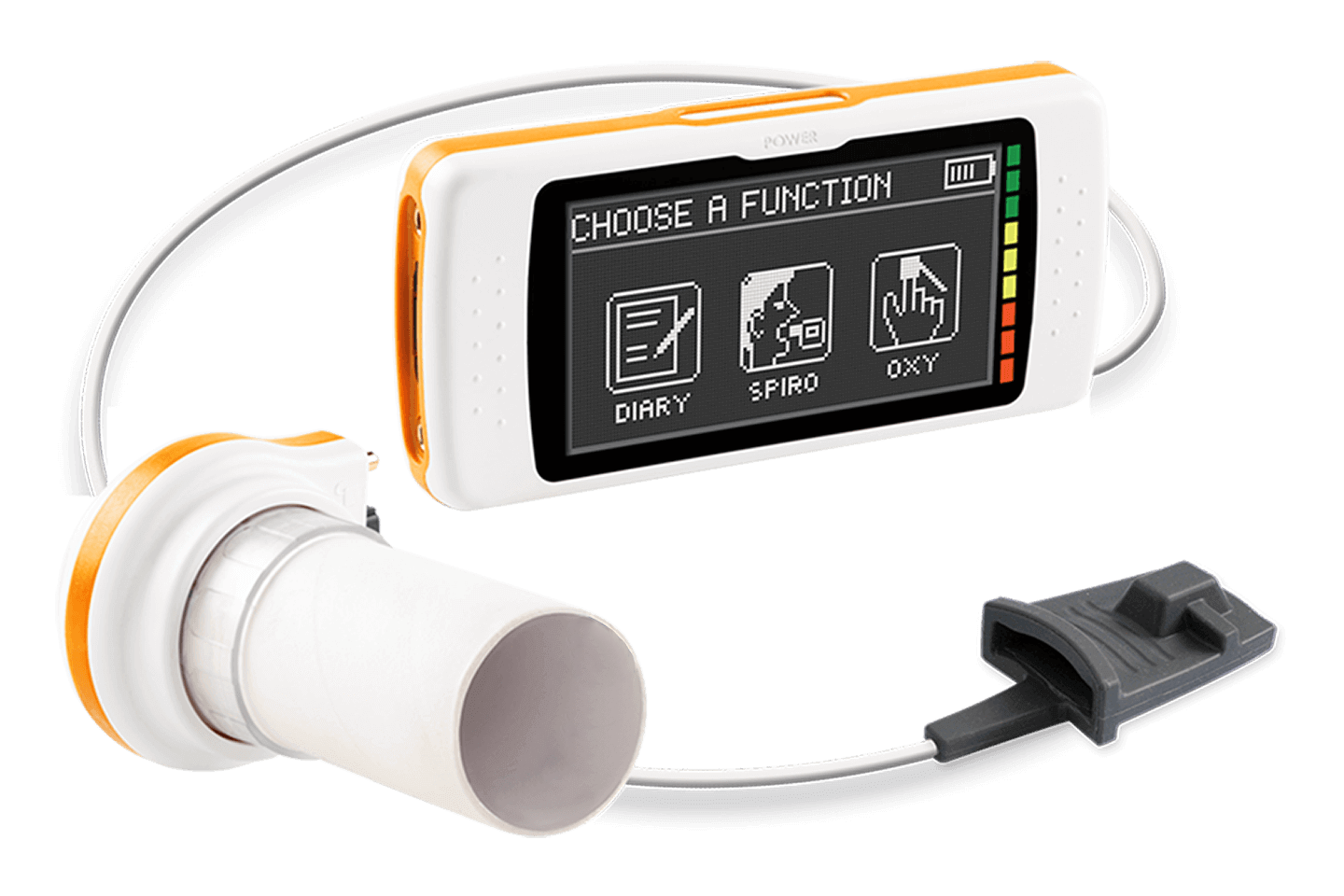
Spiromètre à écran tactile et oxymètre 3D
