


ESI is the outcome of clinical research aimed to evaluate the relative contribution of emphysema to the airflow obstruction measured by standard spirometry. The expiratory airflow obstruction of patients with Chronic Obstructive Pulmonary Disease (COPD) results in morphologic changes of the flow/volume curve.
ESI method, based on fluid-dynamic modeling of the airways, describes the shape of the expiratory fraction of the flow/volume curve whose inflexion is widely held as an index of emphysema presence.

ESI

The mathematical model permits to evaluate the contribute of emphysema to the measured obstruction using as input variables: Peak Expiratory Flow (PEF), Forced Vital Capacity (FVC) and the Forced Expiratory Flows (FEF) at 25%, 50% e 75% of FVC. All input variables are in absolute value.
The computation, indeed, being based only on the morphology of the flow/volume curve of each subject, independently of its own ethnic and anthropometric characteristics, does not necessitate of input variables expressed as percent predicted of a reference population.
The accuracy of the method has been initially evaluated in 194 patients with COPD in which the presence and severity of emphysema has been objectively determined by pulmonary function testing including static lung volumes and diffusing capacity. All patients underwent also inspiratory and expiratory chest CT to assess quantitatively the parenchymal destruction due to emphysema by using three different recently developed softwares: VIDA (University of Iowa), Imbio LDA (Harvard University) e CALIPER (Mayo Clinic) (1).
ESI methodology has been further validated in 5936 subjects of the NIH financed COPDGene study in whom standard spirometry and inspiratory-expiratory CT were obtained in the same day. The results obtained in the multiethnic American population of smokers, ex-smokers and COPD were fully comparable to those obtained in the Italian patients with COPD (2).
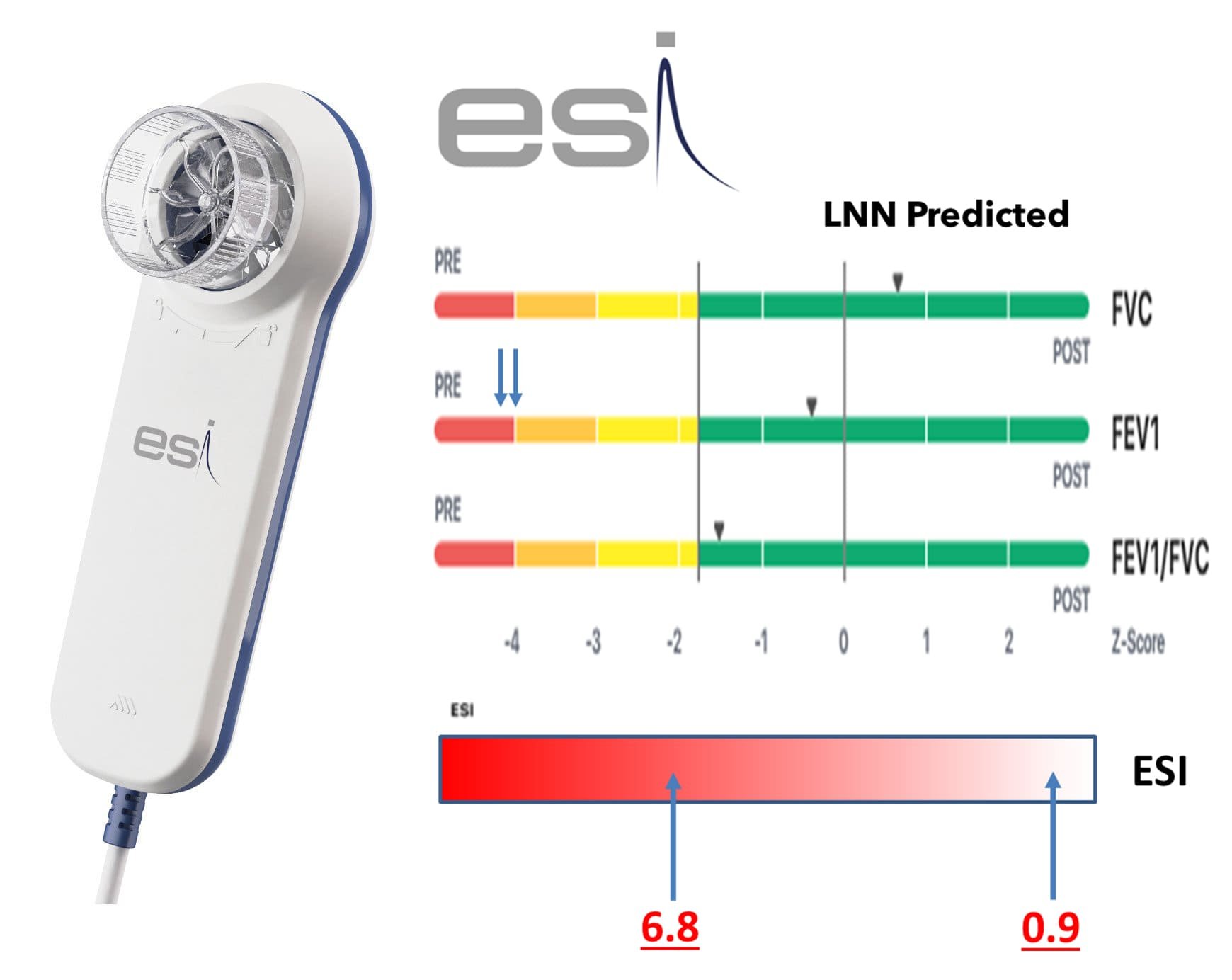
ESI indicates the degree of emphysema in a scale ranging from 0 to 10. ESI values are highly correlated with the levels of parenchymal destruction measured by CT (p ❮ 0.001). A recent multicentric study showed that ESI may greatly differ in patients with similar levels of obstruction allowing identification of the relative contribute of emphysema to the airflow obstruction measured by spirometry (3).
An epidemiologic retrospective study of the geriatric Swedish population showed that one unit increase in ESI increased the hazard of 10-year all-cause death by 20% (p=0.0002) and the hazard of respiratory death by 57% (p ❮ 0.0001) (4).
In the same population ESI is the only variable among those considered (age, male sex, cigarette smoking, FEV1, ESI) that specifically predicts respiratory death.
The addition to spirometry of the novel functional parameter ESI allows to define in each patient what portion of the airflow obstruction measured by the standard spirometric indexes has to be attributed to inflammatory narrowing of the conductive airways (chronic bronchitis, bronchiolitis, small airway disease) or to emphysematous destruction of lung parenchyma.
Patients with the same obstruction (FEV1) level, but different ESI value should be considered different from the pathophysiologic, therapeutic and prognostic point of view. See the accompanying figure (Figure1) referring to two patients with 45% and 44% FEV1 and very different values of ESI. A standard spirometry with ESI computation allows obtaining clinical information comparable to that obtainable with complete pulmonary function testing and in close agreement with the parenchymal destruction quantitatively evaluated by chest CT.
ESI could also be of great relevance for the evaluation of the results of large scale epidemiologic, clinical, and pharmacologic trials in which, usually, standard spirometry is the only available pulmonary function examination.
ESI adds to standard spirometry the ability to discriminate whether emphysema or conductive airway disease is the predominant mechanism of airway obstruction and, consequently, it could be a valuable means in clinical practice in terms of more individualized prognosis and treatment alternatives.
In this connection, ESI could be considered a simple tool to advance Respiratory Medicine towards the new concept of 4P Medicine (Preventive, Predictive, Precise, Personalized).
Indeed, ESI could be used to incentivize smoking cessation (Preventive), to derive prognostic information (Predictive), to identify the main mechanism underlying airway obstruction (Precise), and to select the most individualized pharmacologic treatment (Personalized).
As an exclusive support of this revolutionary achievement in clinical, therapeutic, and prognostic fields are the latest generation spirometers of MIR Plus line, the only ones in the national and international market that will implement this parameter by adding to Spirometry the power to support the diagnosis of emphysema by means of numerical values comparable with the measurements obtained by CT analysis and in line with the results published in scientific journals.